Bone and Joint infections
Osteomyelitis
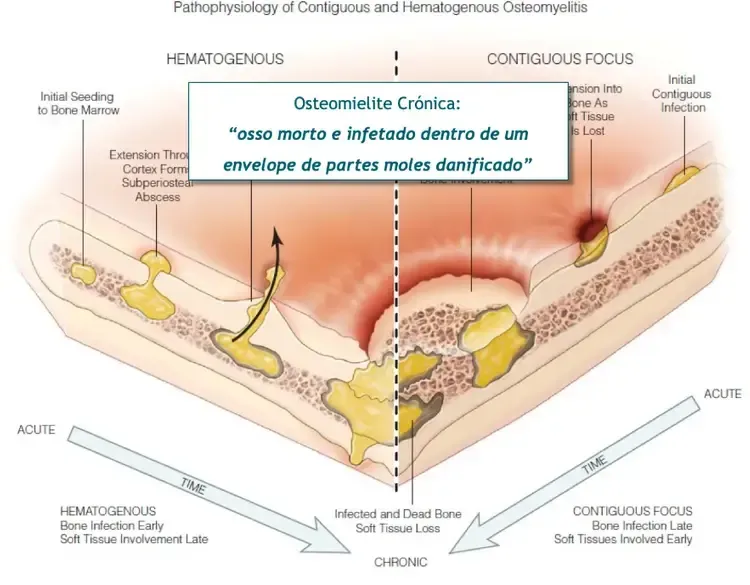
It is often a problem of bone infection but also of the soft tissues around it.
LESÕES
DO JOELHO
INFEÇÕES OSTEOARTICULARES

Bone and Joint infections

Osteomyelitis infection
What is Osteomyelitis?
Osteomyelitis is an infection of the bone, characterized by inflammation and destruction caused by infecting bacteria. Regardless of its origin, chronic osteomyelitis consistently affects one or more areas of the bone and, in advanced stages, may involve the surrounding soft tissues, including the periosteum, muscle, and skin.
Causes
Osteomyelitis can develop from any situation that allows bacteria to enter the bone. Traditionally, hematogenous spread (through the bloodstream) was the typical mode of infection in children, though it is less common today.
Currently, most cases of osteomyelitis are acquired exogenously, usually through a breach in the barrier between the bone and the external environment. The most significant risk factor is open fractures, where the skin is broken, exposing the bone to bacteria.
Surgical interventions for fractures or other pathologies requiring bone surgery (e.g., osteotomies for deformity correction) also pose a risk by exposing bone to potential infection, even in controlled, sterile environments.
Classical risk factors such as obesity, immunosuppression, smoking, and diabetes also contribute to osteomyelitis risk by diminishing the immune system’s effectiveness.
A specific form of osteomyelitis common in diabetic patients originates from an infection in an ulcer bed, progressing from a superficial infection to bone involvement, known as contiguous osteomyelitis.
Symptoms
Symptoms of osteomyelitis vary with the location of the affected bone. Local pain is the primary symptom, which can vary in intensity and may fluctuate. Fever and general malaise are less common and typically occur with exacerbations that have systemic impacts.
Classic signs of inflammation such as redness, warmth, and swelling may or may not be present, depending on the activity level of the infection and the depth of the affected bone.
These signs are more common in superficial bones like the tibia or clavicle and less so in deeper bones like the femur. If near a joint, joint effusion may also be apparent.
In chronic cases, a skin fistula often forms, providing a drainage route for infection between the bone and external surface. This drainage can vary in intensity and may be intermittent.
Diagnosis
Diagnosing osteomyelitis is typically straightforward, characterized by pain and local inflammatory signs. Often, a cutaneous fistula with drainage is present, indicating infection.
Diagnosis is confirmed through imaging techniques such as X-rays, CT scans, and MRIs, alongside evaluations of systemic impacts via blood tests and understanding the type of host affected.
Treatment Options
Treating chronic osteomyelitis usually requires surgical intervention, as antibiotics alone cannot eliminate the bacteria colonizing the bone. The treatment process includes:
1) Surgical debridement of all infected bone, with samples taken for microbiological study to identify infecting bacteria.
2) Filling any voids to prevent them from harboring bacteria.
3) Stabilizing the area if bone continuity is compromised.
4) Ensuring adequate soft tissue coverage, as bone healing and infection resolution are only achievable with healthy surrounding tissues.
5) Administering targeted antibiotics specific to the infecting bacteria.
Treatment must be comprehensive and sequential, addressing both the infection and structural integrity of the bone.



Articulações danificadas por uma prótese são complicações que podem levar a situações muito dolorosas e exigir uma reintervenção cirúrgica para resolver o problema.
Essa é a minha paixão e área de investigação clínica e o principal foco da minha atividade nos últimos anos. Resolver complicações associadas a próteses que não correram bem é a minha grande especialidade
Prof. Dr. Ricardo Sousa
MÉDICO ORTOPEDISTA CIRURGIÃO
Structured and unique approach in Portugal!
Copyright © 2026 Ricardo Sousa Ortopedia All rights reserved
Copyright © 2026 Ricardo Sousa Ortopedia
All rights reserved
Powered by Pointfull.




