Bone and Joint infections
Fracture Related Infection
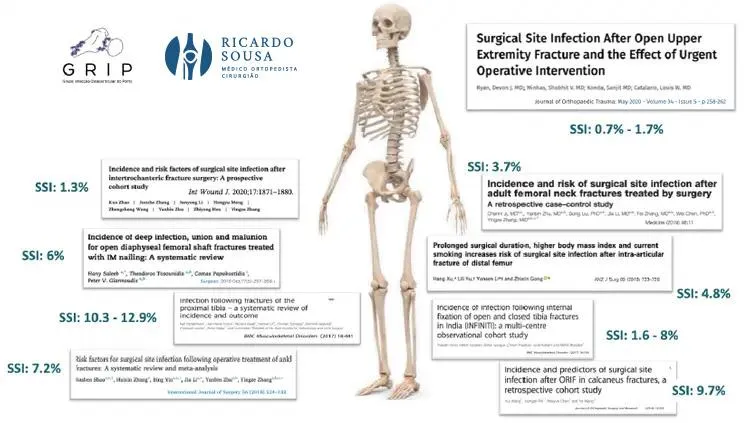
Fracture-related infection is now the most common type of bone infection.
LESÕES
DO JOELHO
INFEÇÕES OSTEOARTICULARES

Bone and Joint infections

Fracture Related Infection
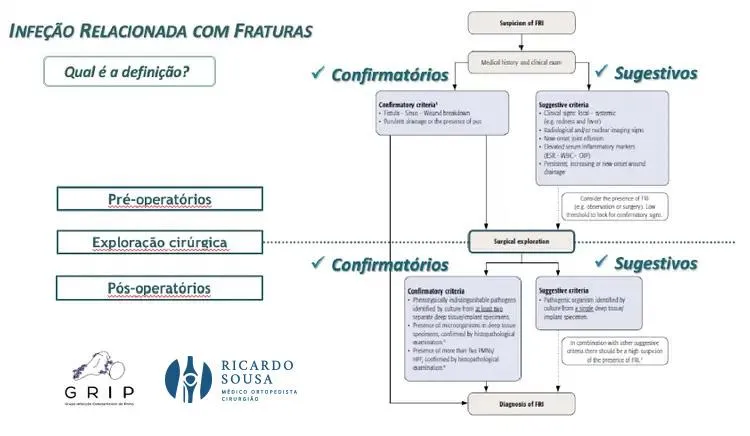
What is a Fracture Related Infection?
Fracture-related infection is now the most common type of bone infection, previously categorized under osteomyelitis.
Although theoretically straightforward to define as an infection that occurs following the treatment of a fracture, in clinical practice, it is often extremely challenging to confirm its presence or absence.
Until very recently, there was no universally accepted definition of the criteria that define this condition.

Causes
The primary risk factor for a fracture-related infection is having sustained an open fracture. These are fractures where there is a wound that disrupts the skin and soft tissue barrier covering the bone, thereby creating a direct link between the external environment and the fracture or its hematoma.
The likelihood of infection also heavily depends on the location of the fracture, with anatomical areas that have less soft tissue coverage, such as the tibia, being at greater risk.
Symptoms
The symptoms of fracture-associated infection vary considerably. They may be pronounced, displaying typical signs of infection such as warmth, redness, intense pain, and pus drainage from the surgical wound in cases with a high bacterial load.
Alternatively, symptoms can be more subtle and thus harder to identify, manifesting as exaggerated pain (hard to differentiate from normal fracture pain) or difficulties in wound healing.
In later stages, the infection may cause failure of the fixation material with osteolysis (bone loss) around the implants or even non-union (pseudoarthrosis) of the fracture.
An enduring warning sign is persistent pain that does not improve significantly over time. In more chronic cases, a fistula— a small, draining wound—may develop on the skin, with variable intensity and intermittency of purulent discharge.
Diagnosis
Initial steps in diagnosing a suspected infection include evaluating the clinical history for risk factors and conducting a thorough physical examination. Indicative signs of infection are purulent drainage from the wound during an acute phase or the presence of a fistula during a chronic phase.
Often, signs are subtler, including exaggerated local pain, joint effusion in fractures involving joints, or indicative changes in radiographs such as fixation material failure, osteolysis, or delayed fracture consolidation. Inflammatory markers in blood tests may or may not show elevation.
Treatment Options
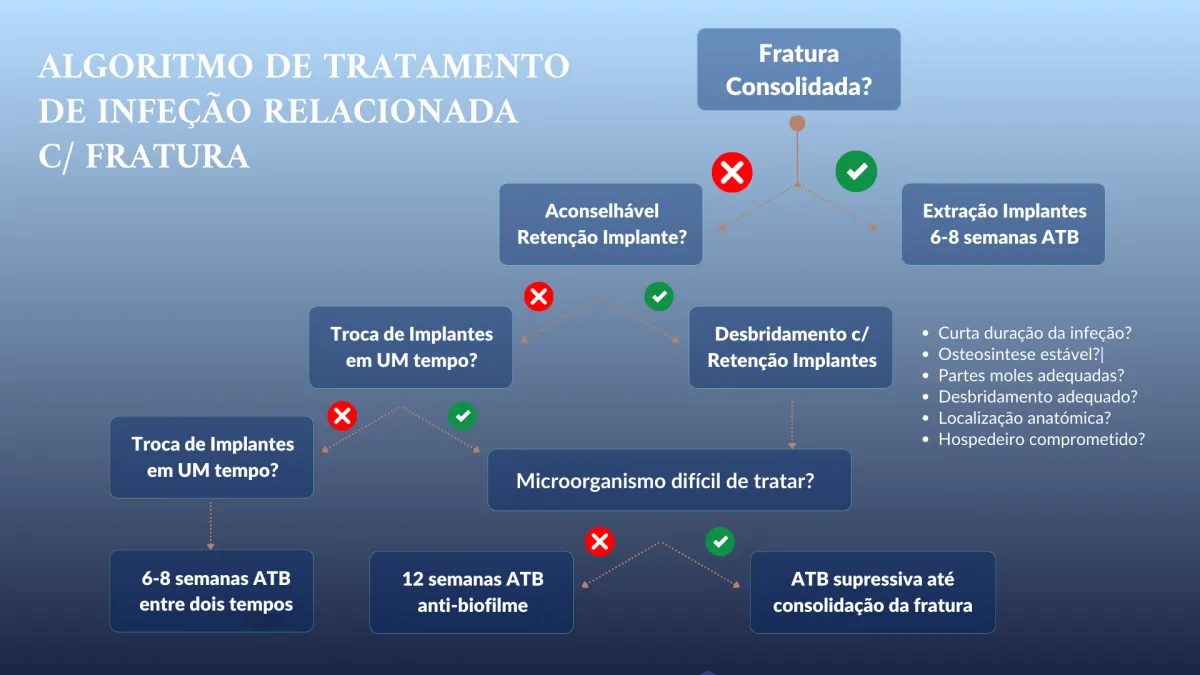
In most cases, treating a fracture-associated infection involves surgical intervention combined with antibiotics targeted at the identified bacteria.
The primary goal, besides eradicating the infection, is to ensure the fracture consolidates properly. Treatment must therefore be tailored to each specific case and depends on whether the fracture has already consolidated, the anatomical location of the fracture, the duration of the infection, and the type of bacteria involved.


Osteomyelitis
It is often a problem of bone infection but also of the soft tissues around it.
Click to find out more information
Copyright © 2026 Ricardo Sousa Ortopedia All rights reserved
Copyright © 2026 Ricardo Sousa Ortopedia
All rights reserved
Powered by Pointfull.




